History of Medicine: Essential Concepts for Reading Comprehension
📋 Overview
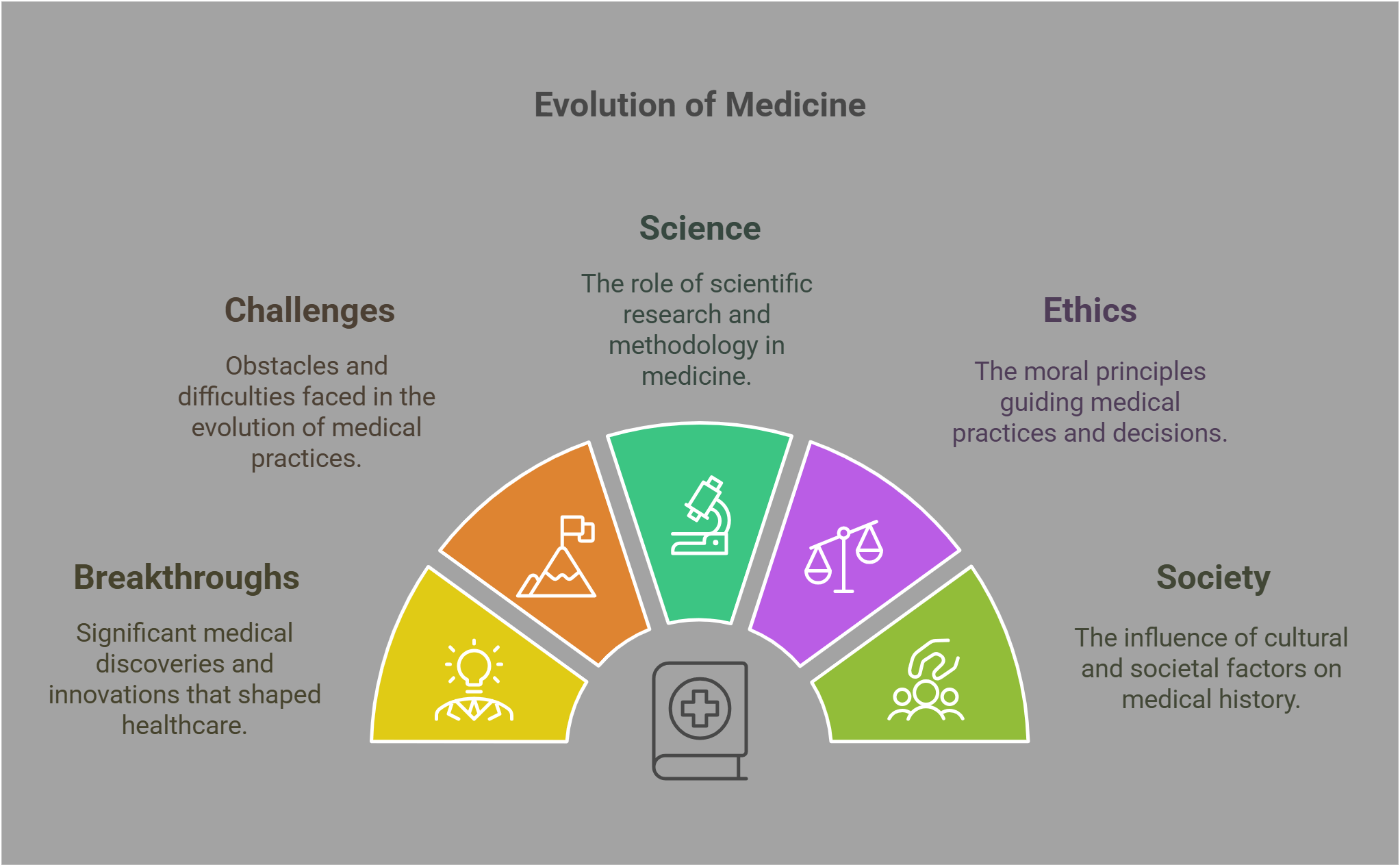
The history of medicine traces humanity’s efforts to understand, prevent, and treat illnesses. It highlights breakthroughs, challenges, and the evolving interplay between science, ethics, and society. From early remedies to modern innovations, each development reflects broader cultural, technological, and philosophical shifts. RC passages on this topic often analyze medical milestones, their impacts, and the lessons they offer. Understanding these concepts enables readers to critically evaluate the journey of medical progress.
🔑 Key Concepts
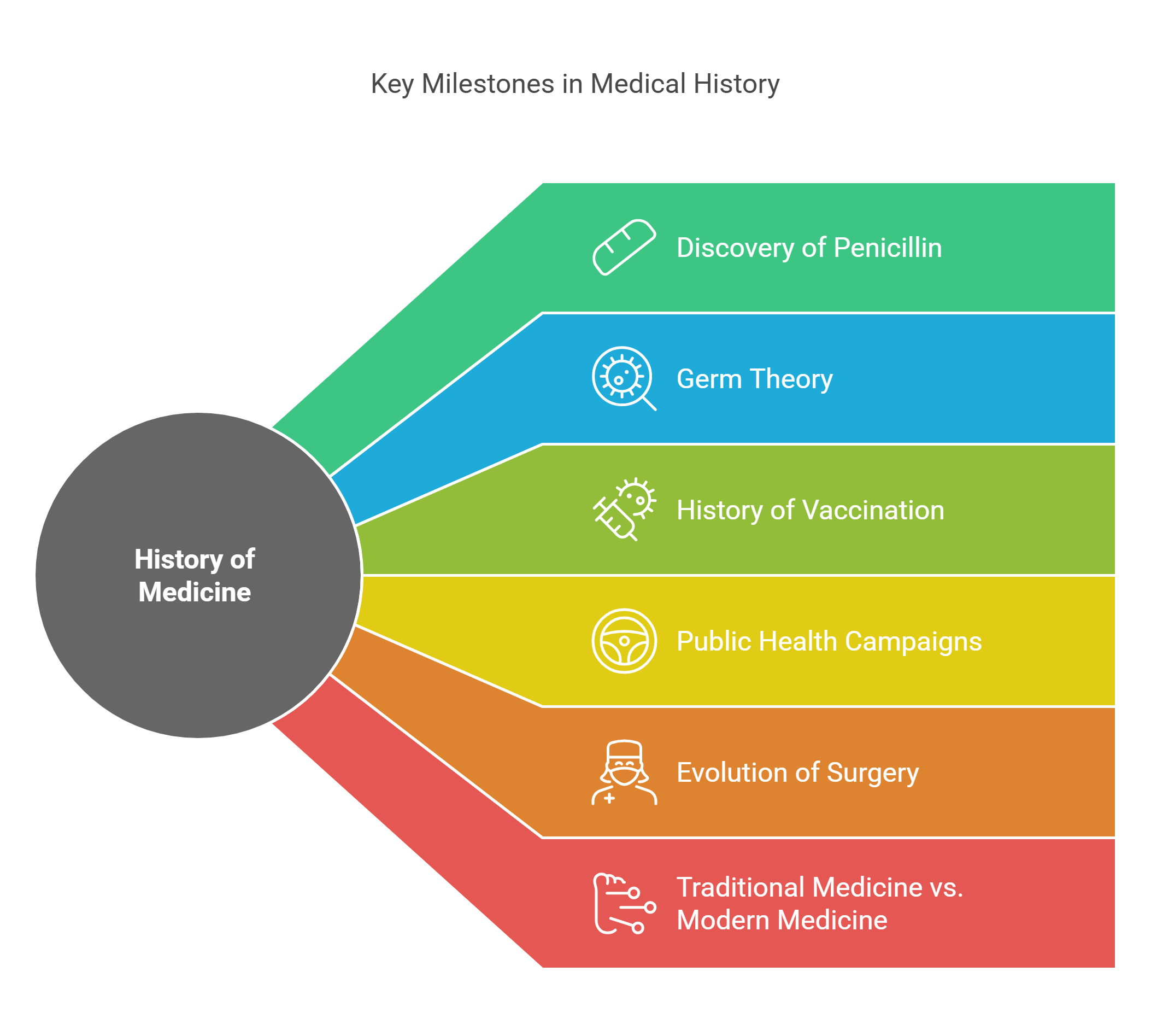
This guide explores the following essential concepts in the history of medicine:
- Discovery of Penicillin
- Germ Theory
- History of Vaccination
- Public Health Campaigns
- Evolution of Surgery
- Traditional Medicine vs. Modern Medicine
- Medical Ethics
- History of Anesthesia
- Mental Health Stigma
- Epidemic Responses
🔍 Detailed Explanations
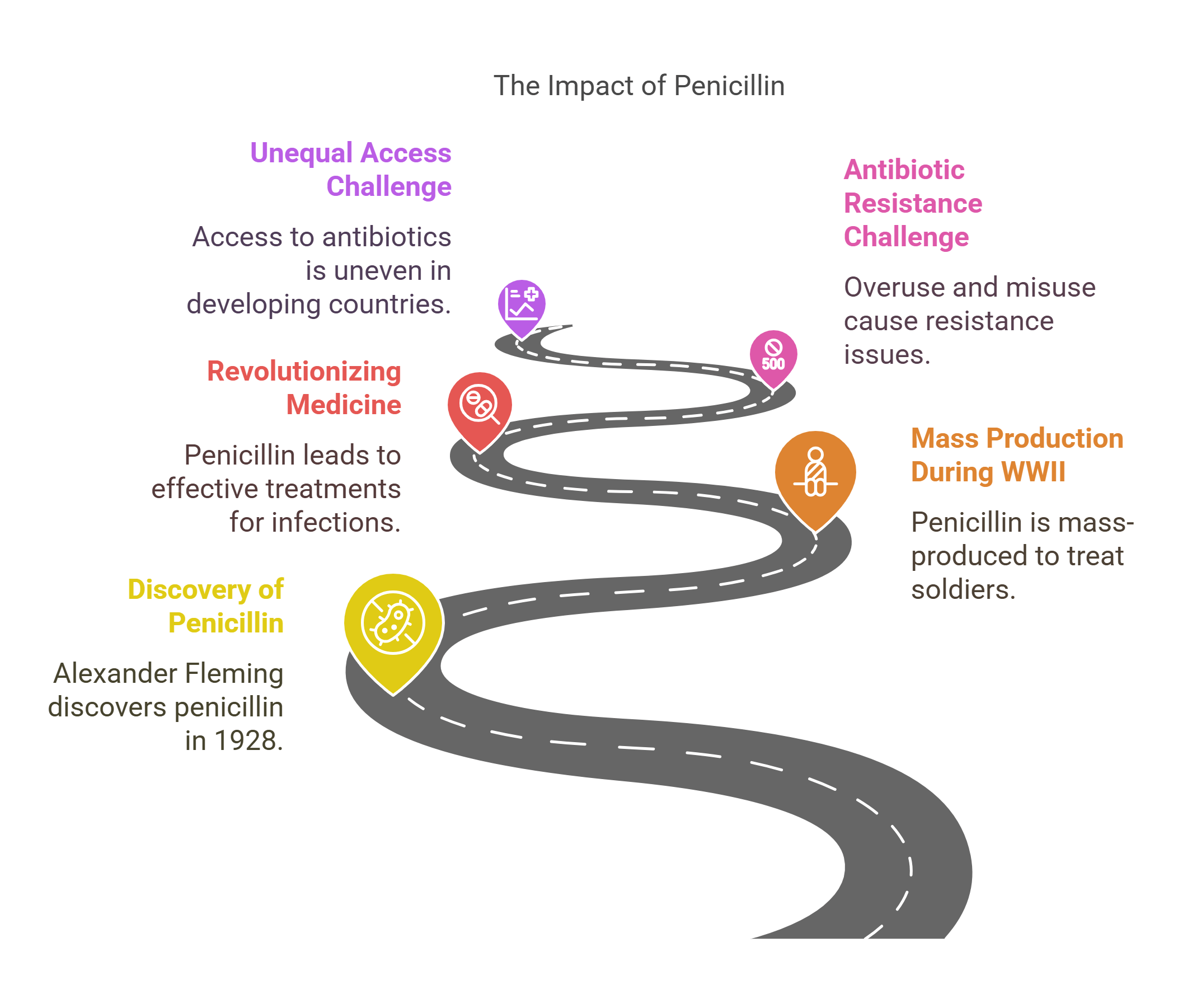
1. Discovery of Penicillin
Penicillin, the world’s first antibiotic, was discovered by Alexander Fleming in 1928 when he observed that mold (Penicillium notatum) inhibited bacterial growth on a culture plate. This breakthrough revolutionized medicine by providing an effective treatment for bacterial infections.
- Key Developments:
- Mass production during World War II saved millions of lives by treating infected wounds and diseases.
- Pioneered the era of antibiotics, leading to treatments for conditions like pneumonia and syphilis.
- Challenges:
- Antibiotic resistance due to overuse and misuse.
- Unequal access to antibiotics in developing countries.
Explained Simply: Penicillin is like a miracle cure that turned once-deadly infections into treatable conditions.
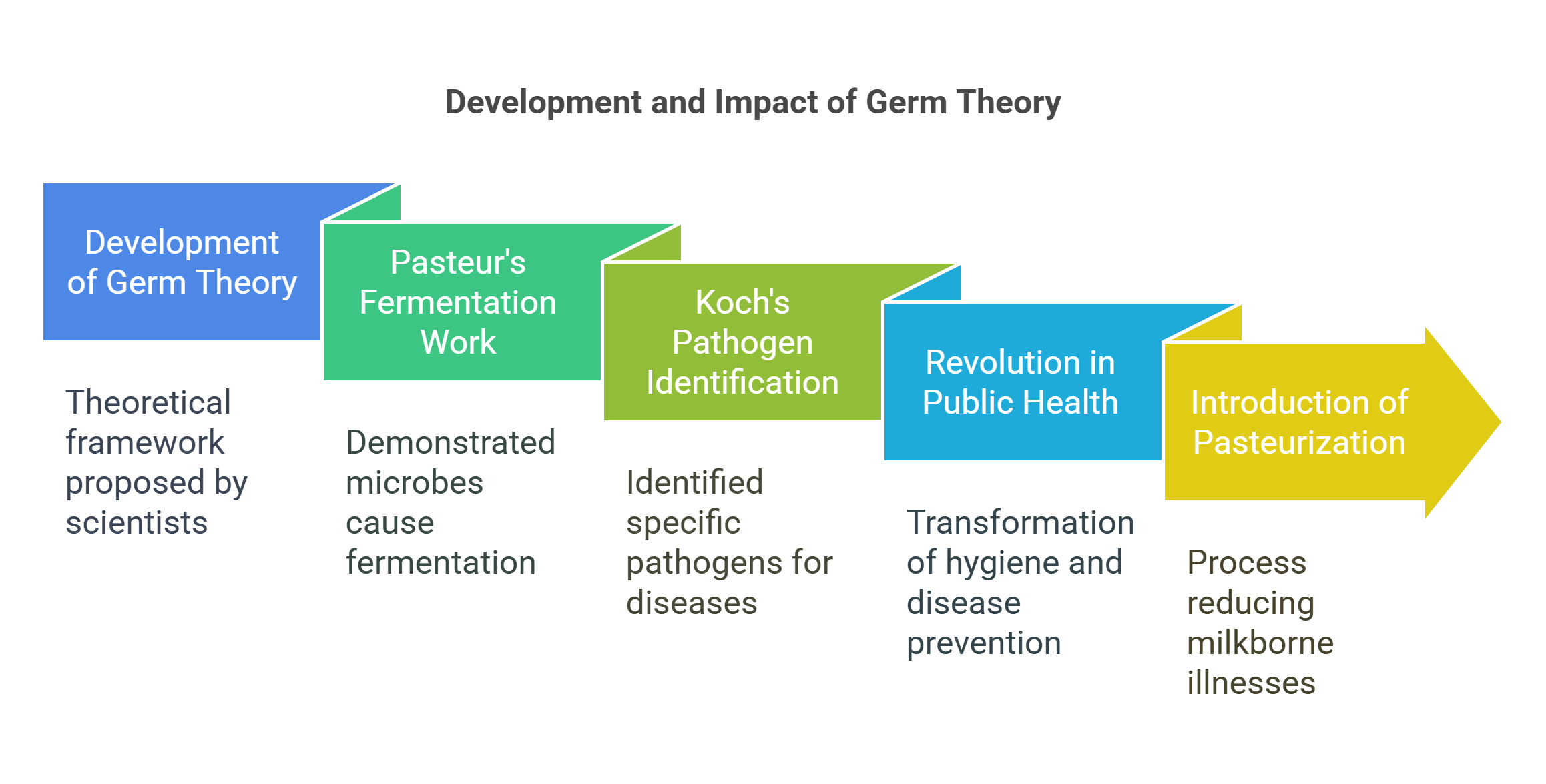
2. Germ Theory
Germ theory, developed in the 19th century, proposed that microorganisms cause disease. This shifted medical understanding from miasma theory (bad air) to microbial causes, transforming hygiene and disease prevention.
- Key Figures:
- Louis Pasteur: Demonstrated that microbes cause fermentation and spoilage, extending the concept to human diseases.
- Robert Koch: Identified specific pathogens for diseases like tuberculosis and cholera.
- Impact:
- Revolutionized public health through sanitation practices, sterilization in surgery, and vaccination development.
Example: The introduction of pasteurization drastically reduced illnesses caused by contaminated milk.
Explained Simply: Germ theory is like discovering invisible invaders that cause sickness, allowing us to fight them effectively.
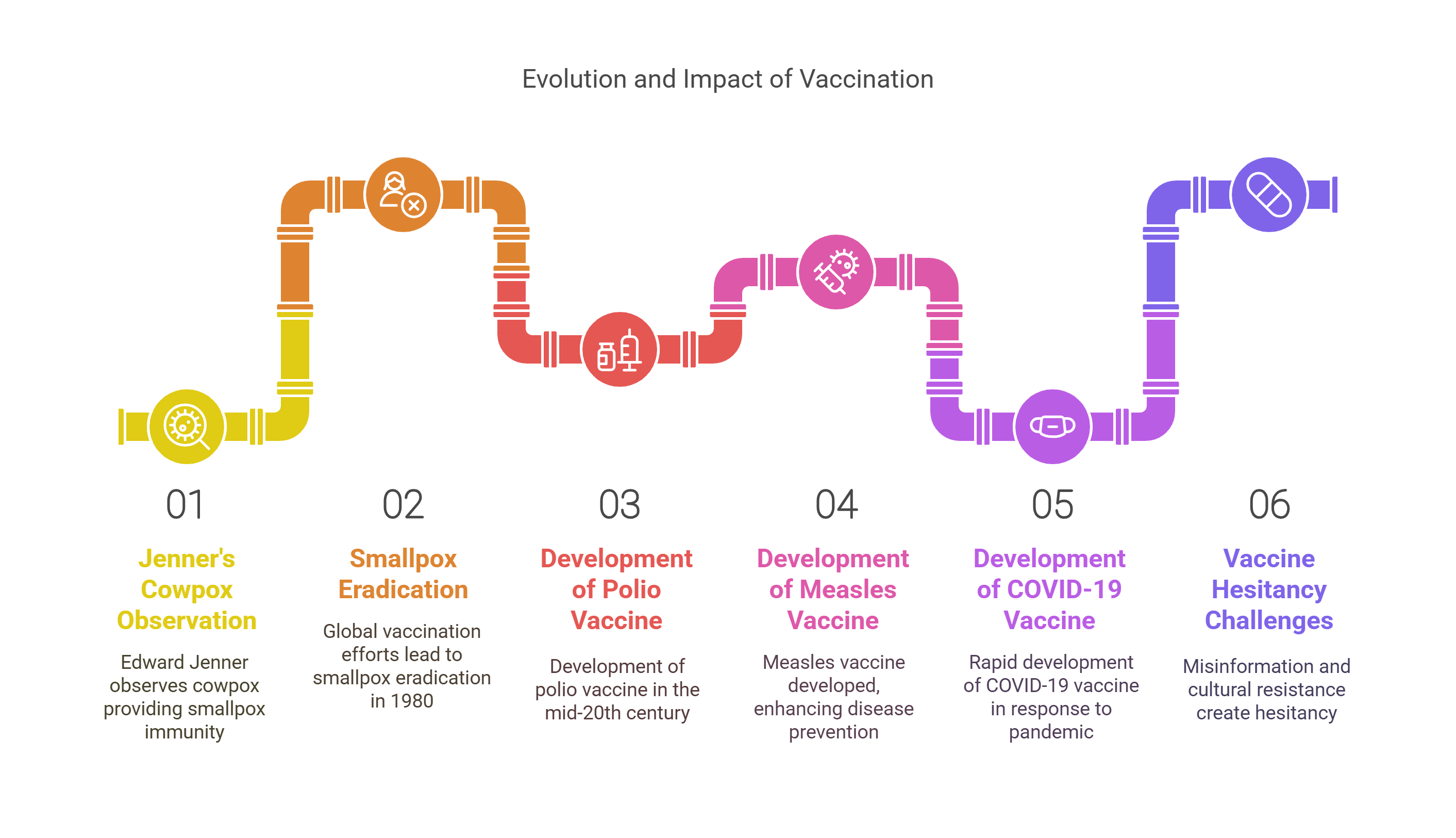
3. History of Vaccination
The concept of vaccination dates back to Edward Jenner in 1796, who observed that exposure to cowpox provided immunity to smallpox. This practice evolved into one of the most effective tools for preventing infectious diseases.
- Key Milestones:
- The eradication of smallpox in 1980 through global vaccination efforts.
- Development of vaccines for polio, measles, and, more recently, COVID-19.
- Challenges:
- Vaccine hesitancy due to misinformation and cultural resistance.
- Ensuring equitable access to vaccines, especially in low-income regions.
Explained Simply: Vaccination is like training your immune system to fight off diseases before they attack.
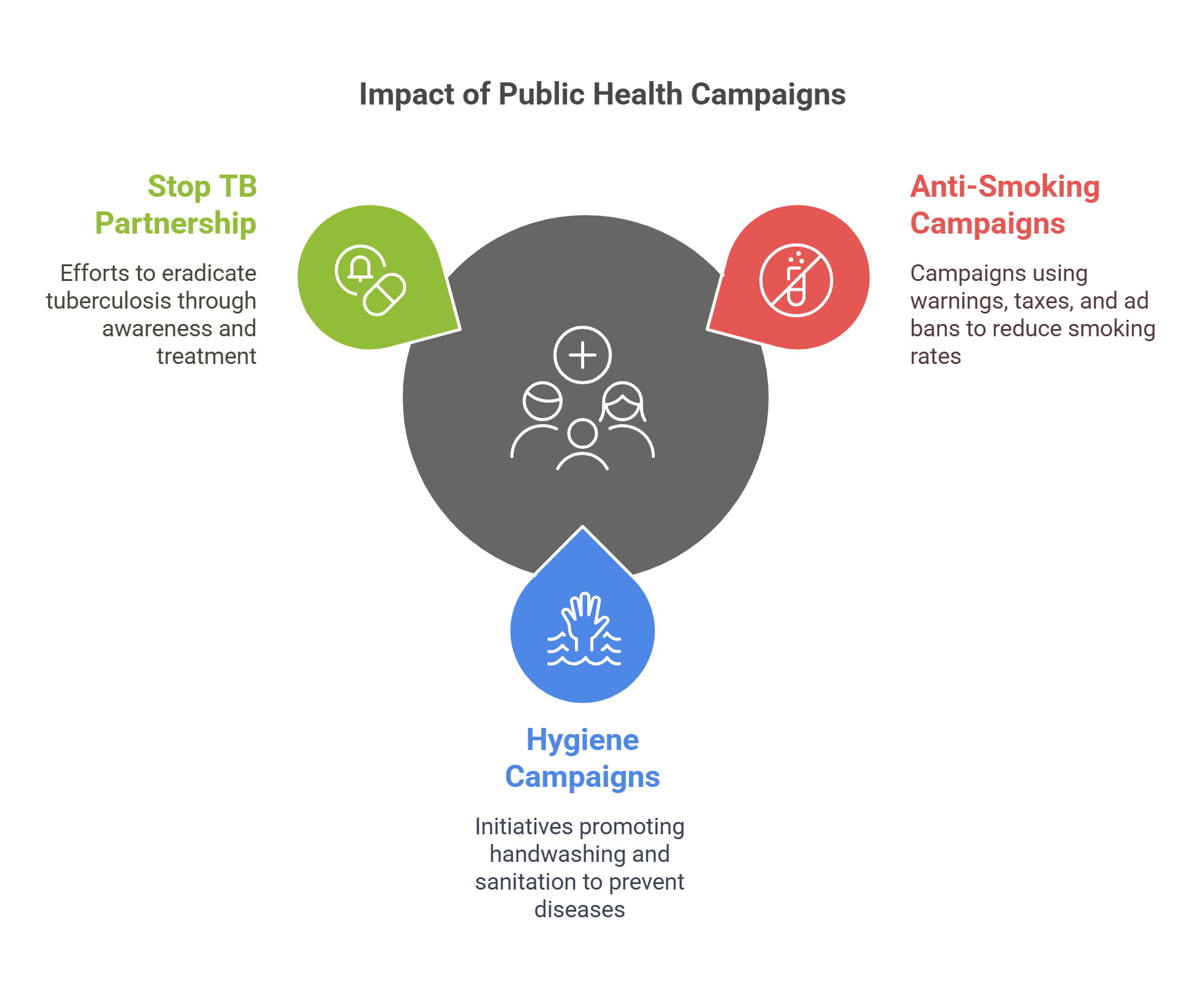
4. Public Health Campaigns
Public health campaigns aim to educate and mobilize communities to prevent diseases and promote healthier lifestyles. These efforts address issues ranging from sanitation to chronic disease prevention.
- Key Campaigns:
- Anti-Smoking Campaigns: Reduced smoking rates through warnings, taxes, and bans on advertisements.
- Hygiene Campaigns: Promoted handwashing and sanitation to curb diseases like cholera.
- Impact:
- Improved life expectancy and quality of life globally.
- Raised awareness about preventable diseases and healthy practices.
Example: The “Stop TB Partnership” campaign focuses on eradicating tuberculosis through awareness and treatment initiatives.
Explained Simply: Public health campaigns are like megaphones for health advice, helping communities stay safe and informed.
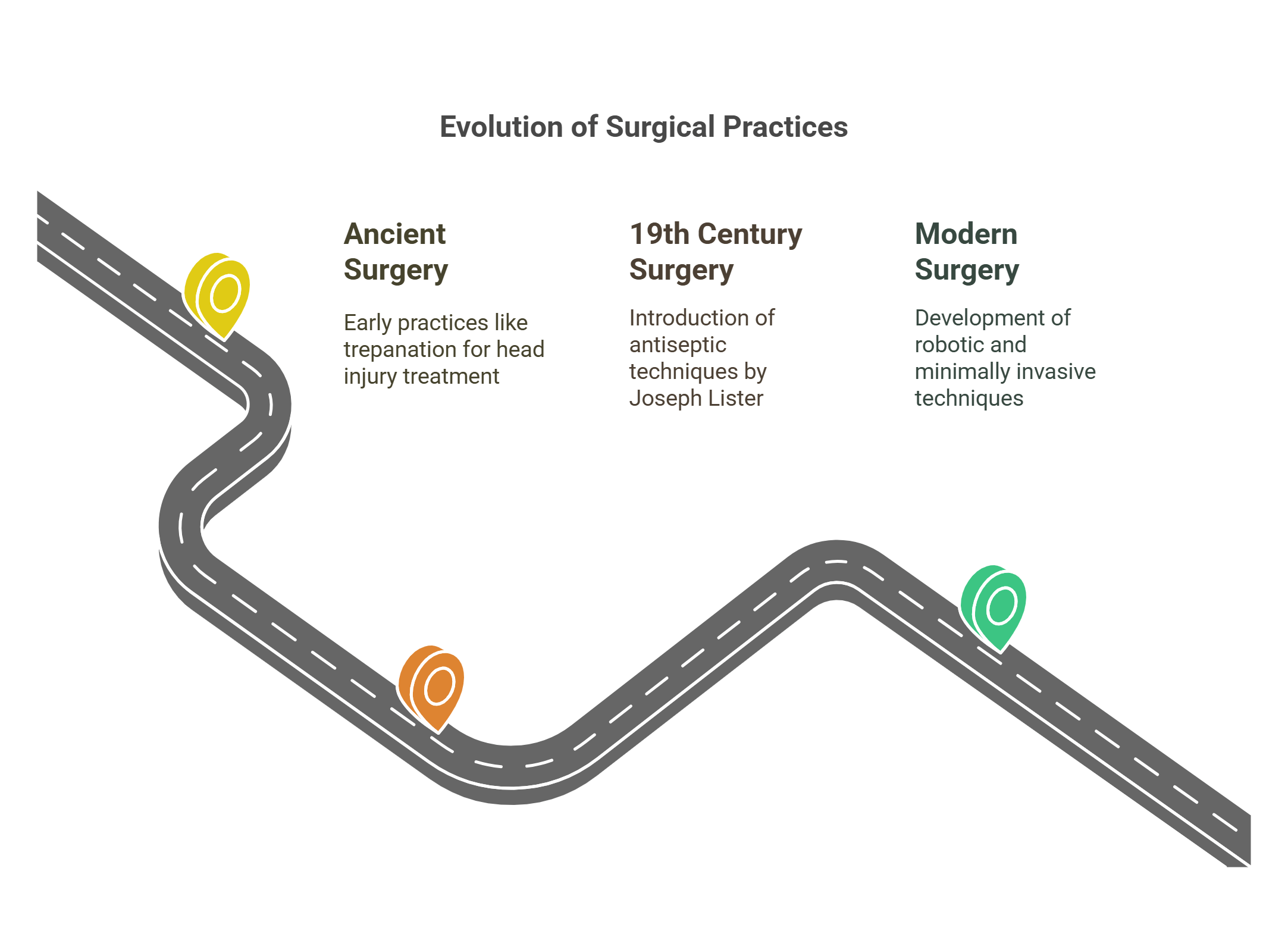
5. Evolution of Surgery
Surgery has evolved from crude practices to precise, lifesaving procedures, driven by advancements in knowledge, tools, and techniques.
- Key Milestones:
- Ancient Surgery: Trepanation (drilling into the skull) for treating head injuries.
- 19th Century: Introduction of antiseptic techniques by Joseph Lister reduced post-surgical infections.
- Modern Surgery: Robotic and minimally invasive techniques improve precision and recovery times.
- Challenges:
- Access to skilled surgeons and modern facilities remains limited in many regions.
- Balancing innovation with patient safety and ethical concerns.
Explained Simply: Surgery is like turning a risky gamble into a refined science, saving lives with precision.
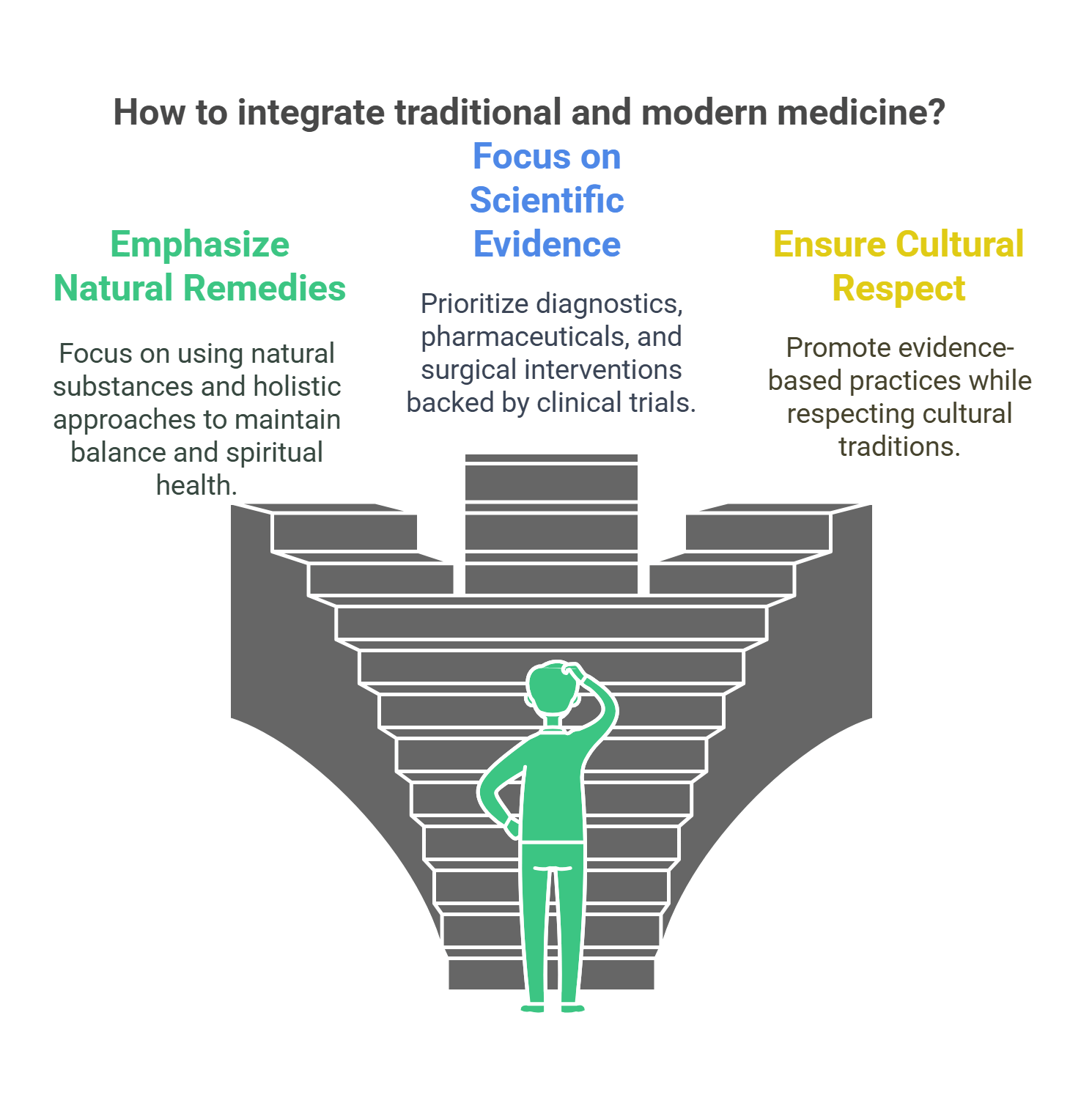
6. Traditional Medicine vs. Modern Medicine
Traditional medicine encompasses healing practices rooted in cultural traditions, often using natural remedies and holistic approaches. Modern medicine relies on scientific research, evidence-based practices, and advanced technologies.
- Traditional Medicine:
- Utilizes natural substances like herbs and minerals.
- Emphasizes balance in the body (e.g., Traditional Chinese Medicine’s yin and yang).
- Often intertwined with spiritual beliefs.
- Modern Medicine:
- Focuses on diagnostics, pharmaceuticals, and surgical interventions.
- Relies on clinical trials and regulatory oversight.
- Advances in biotechnology and genetics drive innovation.
- Challenges:
- Integrating traditional practices into modern healthcare without compromising safety.
- Ensuring cultural respect while promoting evidence-based practices.
Example: Ayurvedic treatments for stress are sometimes incorporated into modern wellness programs.
Explained Simply: Traditional medicine is like wisdom passed down through generations, while modern medicine is like solving health puzzles with science.
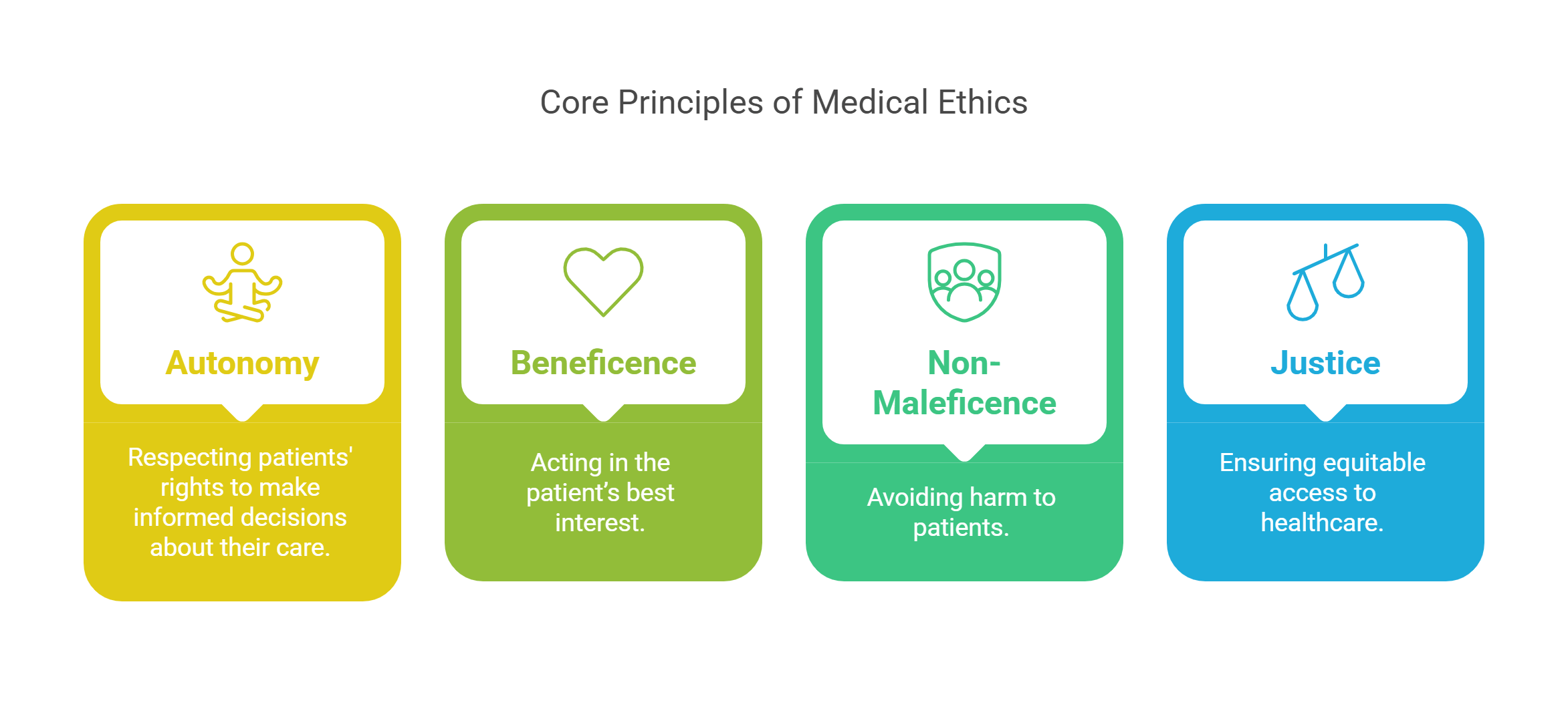
7. Medical Ethics
Medical ethics governs the moral principles guiding healthcare practices, ensuring patient rights, safety, and dignity. It balances technological possibilities with humanity’s values and responsibilities.
- Core Principles:
- Autonomy: Respecting patients’ rights to make informed decisions about their care.
- Beneficence: Acting in the patient’s best interest.
- Non-Maleficence: Avoiding harm to patients.
- Justice: Ensuring equitable access to healthcare.
- Modern Ethical Dilemmas:
- Balancing privacy with the benefits of data-sharing in electronic health records.
- Debating end-of-life care, such as euthanasia and assisted suicide.
Example: The Tuskegee Syphilis Study remains a cautionary tale about the violation of ethical principles in research.
Explained Simply: Medical ethics is like a moral compass for healthcare, ensuring the journey to healing respects all.
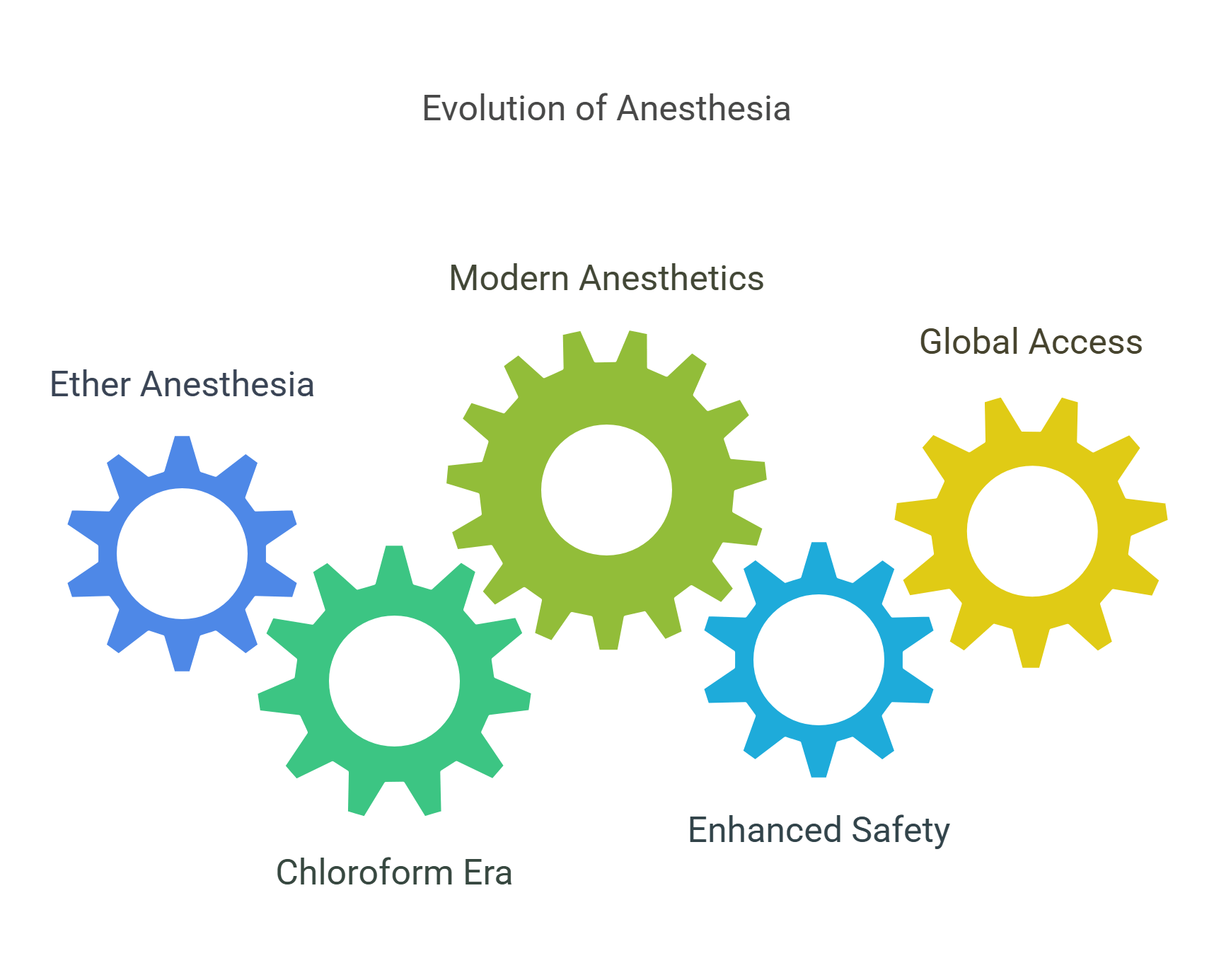
8. History of Anesthesia
Anesthesia revolutionized surgery by allowing pain-free procedures, enabling more complex and prolonged operations.
- Key Milestones:
- 1846: William T.G. Morton demonstrated ether anesthesia for surgery.
- Chloroform: Popularized in the 19th century but later replaced due to safety concerns.
- Modern Anesthetics: Include general, regional, and local options tailored to patient needs.
- Impact:
- Reduced fear of surgery, making life-saving procedures more accessible.
- Improved patient safety with advancements in monitoring and techniques.
- Challenges:
- Managing risks of adverse reactions and complications.
- Ensuring access to safe anesthesia in resource-limited settings.
Explained Simply: Anesthesia is like a pause button for pain, giving surgeons the freedom to heal without causing suffering.
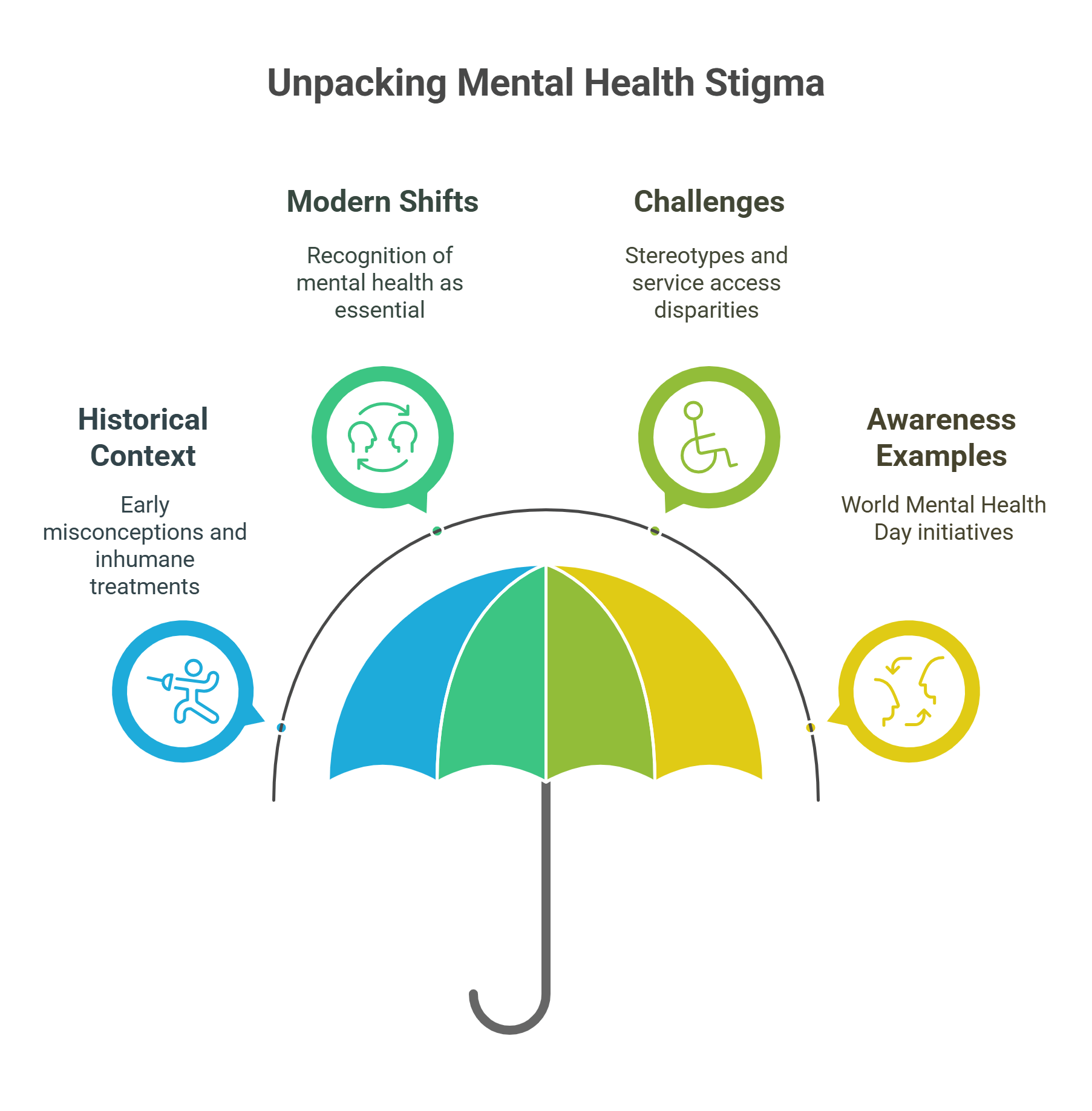
9. Mental Health Stigma
The stigma surrounding mental health has historically marginalized individuals with mental illnesses, hindering treatment and societal acceptance.
- Historical Context:
- Early approaches often treated mental illness as supernatural or moral failure.
- Asylums in the 19th century were often overcrowded and inhumane.
- Modern Shifts:
- Increased recognition of mental health as part of overall well-being.
- Advocacy for therapy, medication, and community support as effective treatments.
- Challenges:
- Persistent stereotypes discourage individuals from seeking help.
- Unequal access to mental health services exacerbates disparities.
Example: World Mental Health Day raises awareness and combats stigma through education and advocacy.
Explained Simply: Addressing mental health stigma is like shining a light on hidden struggles, making help and healing accessible.
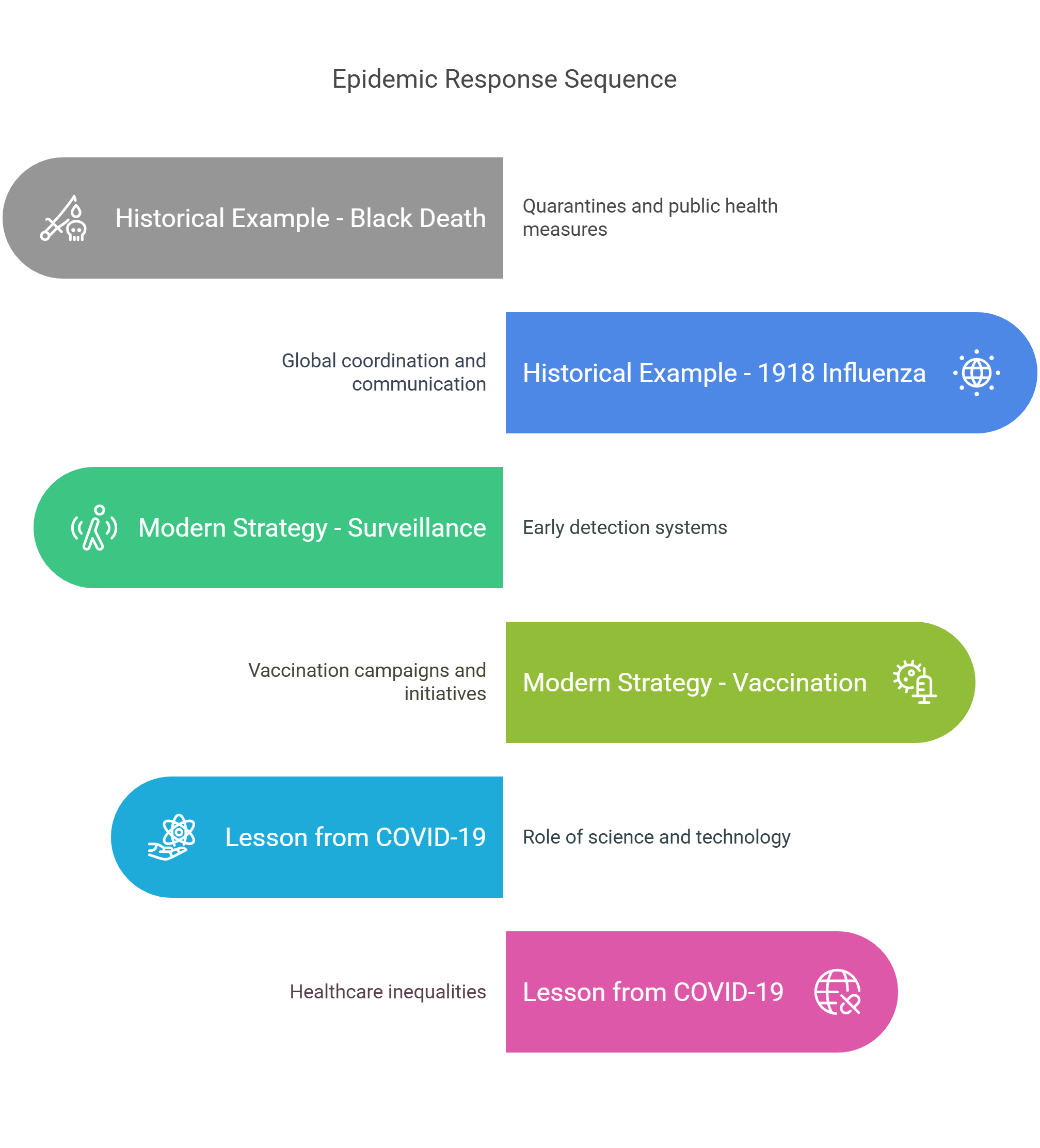
10. Epidemic Responses
Epidemic responses involve coordinated efforts to control and mitigate outbreaks of infectious diseases, combining medical, social, and political measures.
- Historical Examples:
- The Black Death (14th Century): Quarantines and rudimentary public health measures slowed its spread.
- 1918 Influenza Pandemic: Demonstrated the importance of global coordination and public communication.
- Modern Strategies:
- Surveillance and early detection systems (e.g., WHO’s Epidemic Intelligence Service).
- Vaccination campaigns, social distancing, and public awareness initiatives.
- Lessons from COVID-19:
- Highlighted the role of science and technology in managing pandemics.
- Exposed inequalities in healthcare access and global vaccine distribution.
Explained Simply: Epidemic responses are like firefighting for health crises—swift action can save lives and prevent catastrophe.
✨ Conclusion
The history of medicine showcases humanity’s relentless pursuit of healing, revealing a journey of discovery, adaptation, and ethical challenges. By exploring concepts like vaccination, medical ethics, and epidemic responses, readers can critically analyze RC passages and appreciate the profound impact of medicine on society.










